CREËER RUIMTE VOOR ZORG
Thuismonitoring voor ziekenhuizen, huisartsen en de regio
Vertrouwd door toonaangevende zorgorganisaties















Betere én efficiëntere zorg in een handomdraai
Met Luscii monitor en begeleid je patiënten veilig op afstand. Bovendien voorkom je onnodige controles en opnames en maak je bedden sneller vrij. Eenvoudig voor patiënt en voor zorgverleners. Één app voor al je ziektebeelden, direct geïntegreerd in je EPD. In een handomdraai geïmplementeerd en al ingezet door 85% van de ziekenhuizen in de dagelijkse zorg voor vele duizenden patiënten.

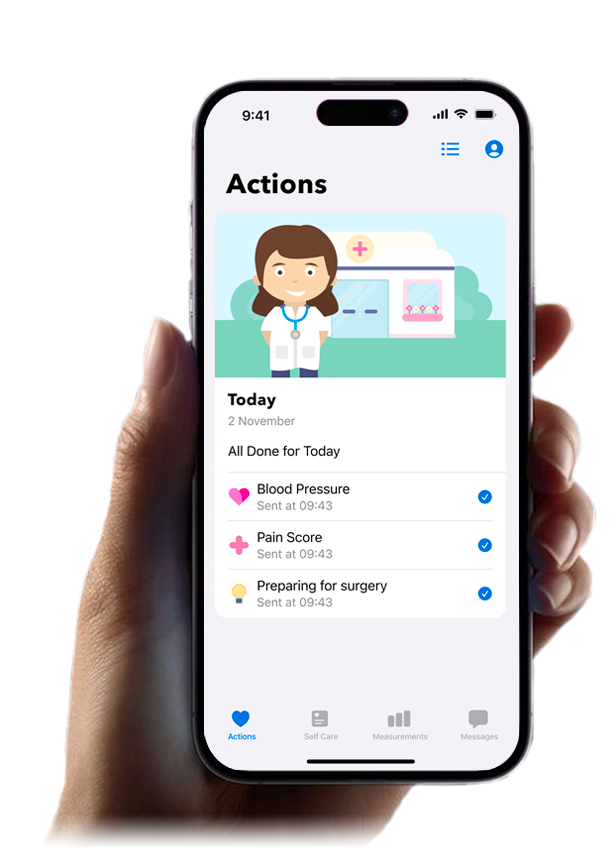
Slimste zorg app beschikbaar
Thuismonitoring voor elk ziektebeeld

Bezoek de Luscii Library
Slimme thuismonitoring programma's voor meer dan 150 ziektebeelden.
Zelf je eigen
programma's creëren
Word Medical Developer
Al gelanceerd in
11 landen wereldwijd
In Europa en Afrika
Eerbetoon aan
een bijzondere vrouw
Het verhaal van Luscii
Stop met
faxen in de zorg
Naadloze (EPD) integratie
Bouw mee aan de toekomst van de zorg
Één thuismonitoring app voor alle ziektebeelden
